QUESTION-1:
4 yo fussy child:
Correct Answer: Epiglottitis
- >3 y.o. kids, peak incidence at 6 y.o.
- purely supraglottic infxn., but will get subglottic edema in 25%
- H.Flu Type B #1, pneumooccus, strep A also
- EMERGENCY, CONTACT “TEAM” ASAP
- Croup seen in younger kids(3 y.o.)-Viral parainfluenza - Normal epiglottis and aryepiglottic folds
Differential Diagnosis:
- Enlarged epiglottis
- Epiglottitis (H. influenza)
- Angioneurotic edema (AD)
- Omega epiglottis (NL variant)
- Trauma/hemorrhage: foreign body, caustic ingestion, hemophilia
- Epiglottic cyst, papilloma
Pearls:
- The lateral radiograph of the neck of a child with epiglotitis may demonstrates enlargement of the epiglottis and thickening of the aryepiglottic folds. Acute epiglottitis is a medical emergency. The most common etiology of acute epiglottitis is Haemophilus influenzae. At least 25% of patients with diagnosed acute bacterial epiglottitis have subglottic edema. Acute epiglottitis is less common than croup but is more dangerous.
- Croup typically occurs in children ages 6 months-3 years, while epiglottitis occurs in children ages 3-6years. For suspected epiglottitis, a portable lateral ST view of the neck should be performed with an ER physician present.
Return Back
Correct Answer Explanation



QUESTION-2:
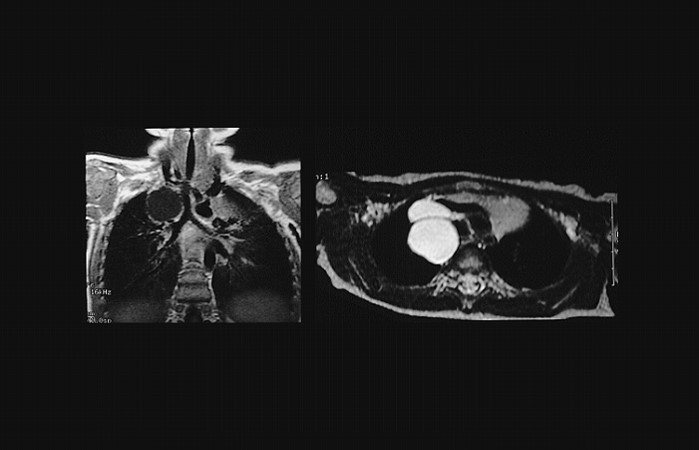
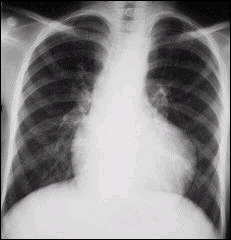
3 yo with incidental mass found:
Correct Answer: Bronchogenic cyst
- MOST COMMON bronchopulmonary foregut malformation
- middle or post.mediastinum
- may compress airway and cause pneumonia
- Mediastinal more common than intrapulmonary
- may communicate with tracheal lumen
Differential Diagnosis:
- Mostly homogeneous
- T1: From low (similar to fluid) to high (due to protein content)
- T2: Usually high signal intensity due to fluid content
Pearls:
- Neuroblastoma most common mediastinal mass in children.
- Neurogenic tumors are the most common mediastinal masses of childhood. Neuroblastoma is much more frequent than ganglioneuroma or ganglioneuroblastoma and usually occurs in children less than 2 years of age. In children, posterior: middle: anterior masses are 40%: 30%:30%. The most common pseudomass in the mediastinum of a child is a normal thymus. Anterior and middle mediastinal masses each comprise 30% of mediastinal masses. Posterior mediastinal masses comprise the other 40% and 90% of those are neurogenic tumors. Peds Requisites,2nd, 52
- “Neurogenic tumors are the most common mediastinal masses of childhood.” Neuroblastoma is much more frequent than other neurogenic tumors.
- Kirks 3rd 790
Return Back
Correct Answer Explanation

QUESTION-3:
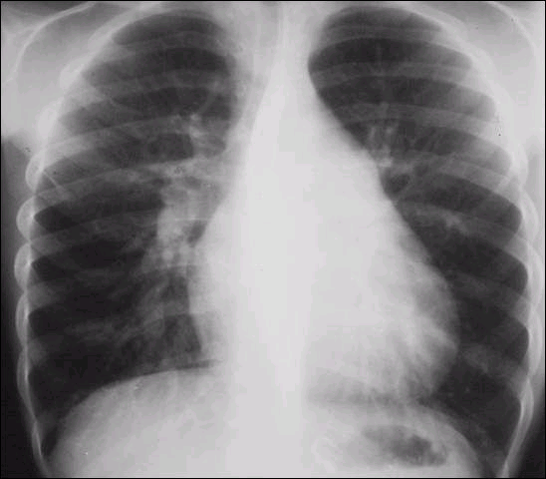
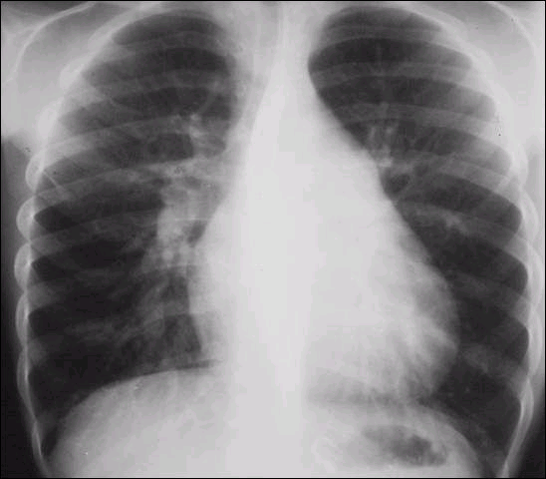
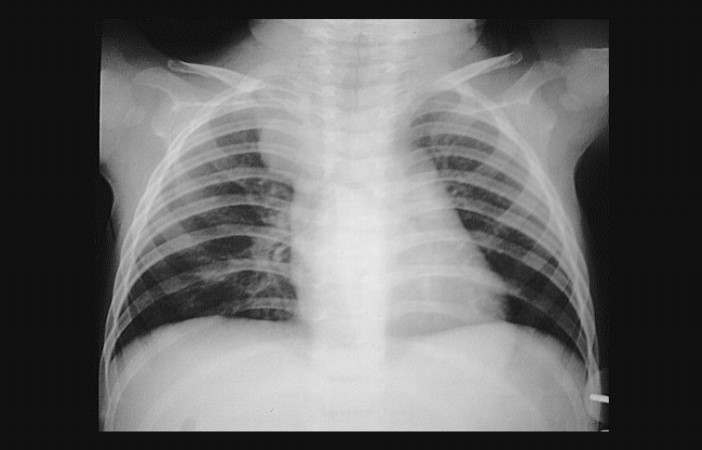
Patient following up with disorder that has known associated with a deletion on chromosome 22q11:
Correct Answer: Tetralogy of Fallot
- Most common cyanotic lesion dx after infancy
- Small PA (BF NL to decreased)
- Image shows a "boot-shaped" heart with an upturned cardiac apex due to right ventricular hypertrophy and concave pulmonary arterial segment.
Differential Diagnosis:
- Pulmonary atresia with a ventricular septal defect
- Absent pulmonary valve syndrome:
- Common arterial trunk
- Double outlet right ventricle
- Truncus arteriosus accounts for up to 2% of congenital cardiac anomalies and is almost always associated with a ventricular septal defect (VSD) to allow circulatory flow circuit completion.
Pearls:
- Tetralogy of Fallot (TOF) is the most common cyanotic CHD of childhood. It consists of the obstructed RV outflow tract, VSD, overriding aorta, and RVH. On CXR there is evidence of decreased pulmonary vascularity. TAPVR and TGA both have increased vascularity and VOG aneurysm results in high output CHF and cardiomegaly.
Primer, p. 109, 118-119, 471
Dähnert 5th p. 604, 650, 651-652, 326-327 - Association of anomalies known as VACTERL.
Most common are cardiac anomalies (VSD, PDA, Tetralogy) and GI anomalies (anal and duodenal atresia)
Others include vertebral anomalies, renal dysplasia and radial ray hypoplasia.
Dähnert 5th 807; Kirks 3rd 843-844
References:
- https://bit.ly/3j7nBNU
Return Back
Correct Answer Explanation

QUESTION-4:
Which of the following is not associated with Down’s syndrome?:
Correct Answer: hypertrophic pyloric stenosis
- Down syndrome is associated with all of the above except pyloric stenosis.
- It is associated with duodenal atresia/ stenosis.
- Dahnert 5th 68
Return Back
Correct Answer Explanation
QUESTION-5:
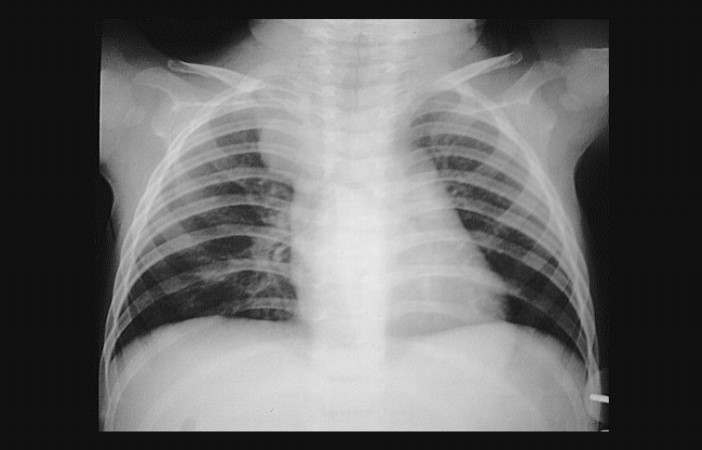
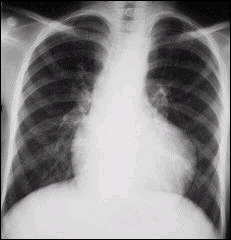
Known acyanotic heart disease:
Correct Answer: Ventricular septal defect
- Most common congenital heart disease, accounting for 20-25% of all CHD
- 4 locations for VSD:
- supracristal
- membranous (the most common - 80%),
- endocardial cushion type (posterior)
- muscular
Differential Diagnosis:
- Radiology
- Large Heart
- Increase Pulm BF
- Enlarged RV, LA and MPA
- hyperinflation
Pearls:
- Algorithmic approach to CHD:
- I. ACYANOTIC A. NORMAL PBF If these lesions are severe can affect PBF Pulm Stenosis, Aortic Stenosis,
- Coarctation (Focal). Diffuse form (Tubular Hypoplasia) can ->CHF B. INCREASED PBF 1. L->R SHUNTS: VSD, ASD, Endocardial Cushion Defect, AP Window Peripheral AVM/ Vein of Galen fistula, Ruptured sinus of Valsalva aneurysm 2. Any cause of failure in heart without shunt: cardiomyopathy, myocarditis, Adriamycin toxicity, sepsis, glycogen storage disease
- II. CYANOTIC = ADMIXTURE lesions A. INCREASED PBF = “R->L SHUNTS” although more blood -> Rt circ due to lower pressure (mnemonic 4TS+CHD) - TGV, TAPVR, Truncus Arteriosus, Tricuspid Atresia with TGV (25%), Single Ventricle, Common Atrium, HLHS, DORV (the last 3 can result in failure also) B. DECREASED PBF = R->L SHUNTS with Pulm Outflow Obstruction so more blood -> Lt (mnemonic TET P) - Tetralogy of Fallot, Ebstein Anomaly, Tricuspid
- Atresia without TGV (75%), Pulmonary Atresia (the 1st 3 are most common, the last 3 cause cardiac enlargement).
References:
- https://bit.ly/2Wx5Kbq
- Gael Lonergan’s excellent handout from AFIP Dähnert 5th 567
Return Back
Correct Answer Explanation