QUESTION-1:
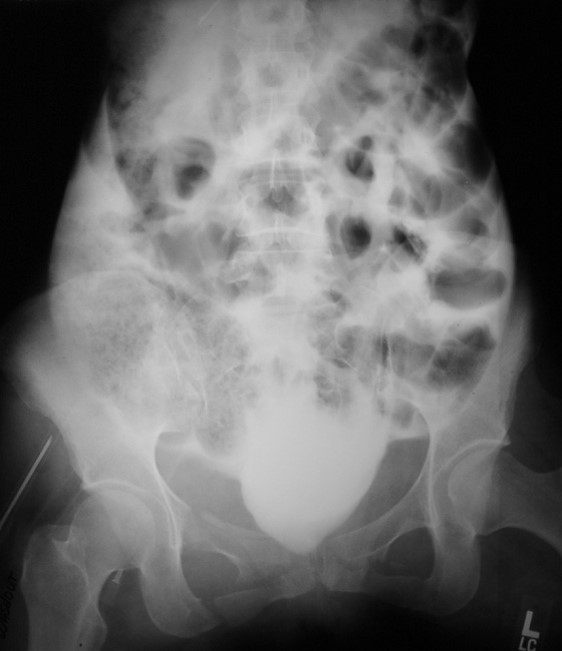
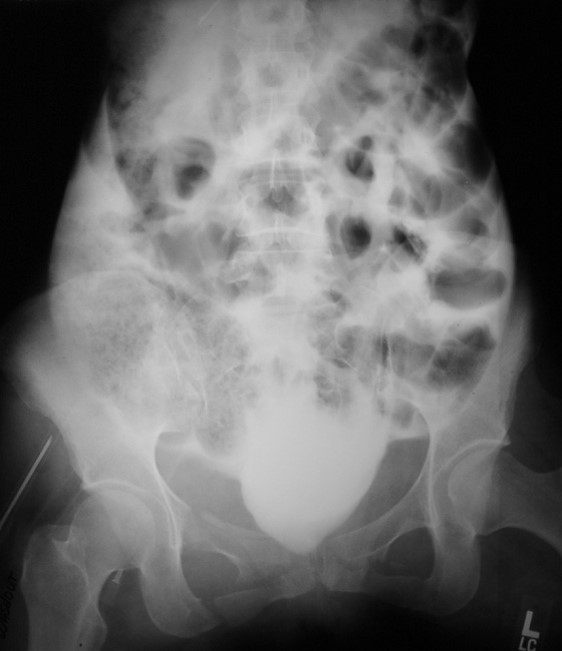
50 yo with hx of hypercalcemia:
Correct Answer: Cortical nephrocalcinosis
- Incidence:5% of all nephrocalcinoses
Cause:
- Acute cortical necrosis
- Chronic glomerulonephritis
- Alport syndrome = hereditary nephritis + deafness
- Congenital oxalosis, primary hyperoxaluria
- Chronic paraneoplastic hypercalcemia
- Rejected renal transplant
US:
- homogeneously increased echogenicity of renal parenchyma > liver echogenicity
Pearls:
- ~20 times less common than medullary nephrocalcinosis.
- Possible other etiologies:
- Renal cortical necrosis: common renal infarction/ischemia
- Sepsis
- Medullary nephrocalcinosis: refers to the deposition of calcium salts in the medulla of the kidney.
Return Back
Correct Answer Explanation




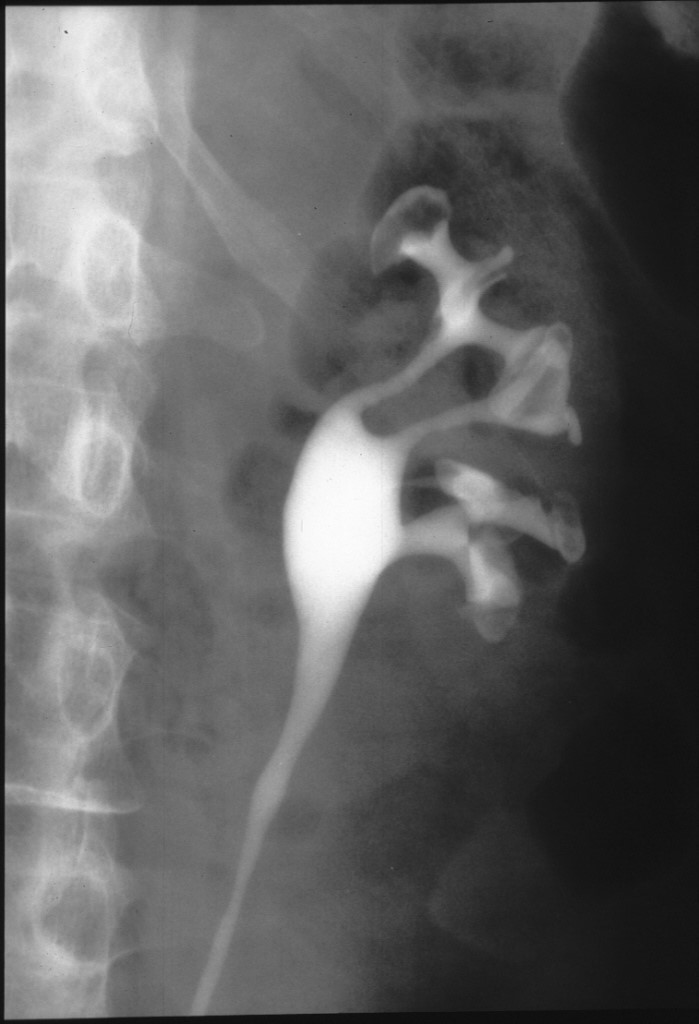
QUESTION-2:
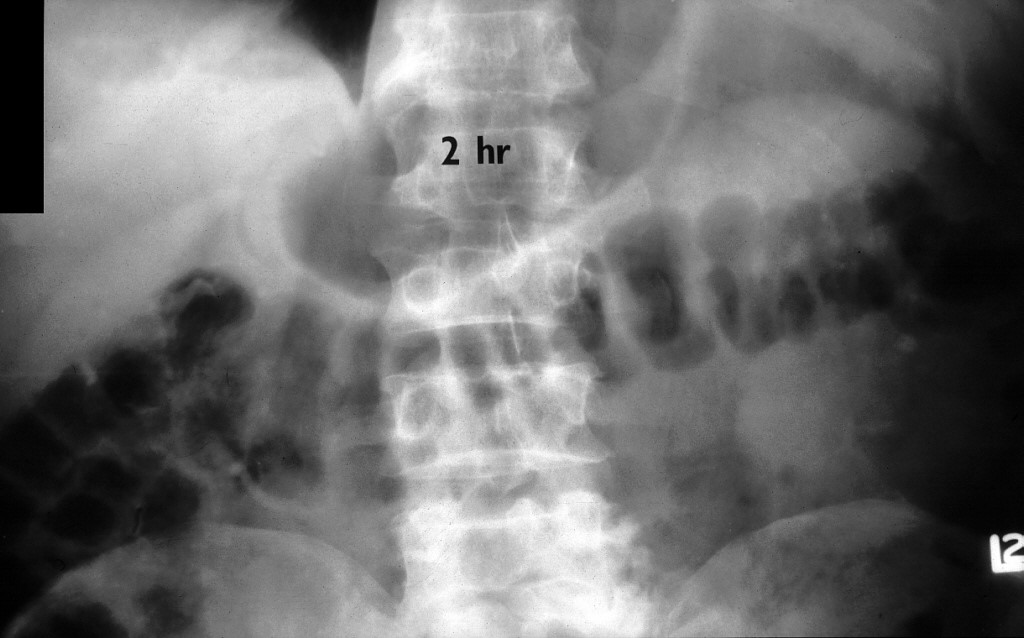
45 yo with fever, chills or rigors:
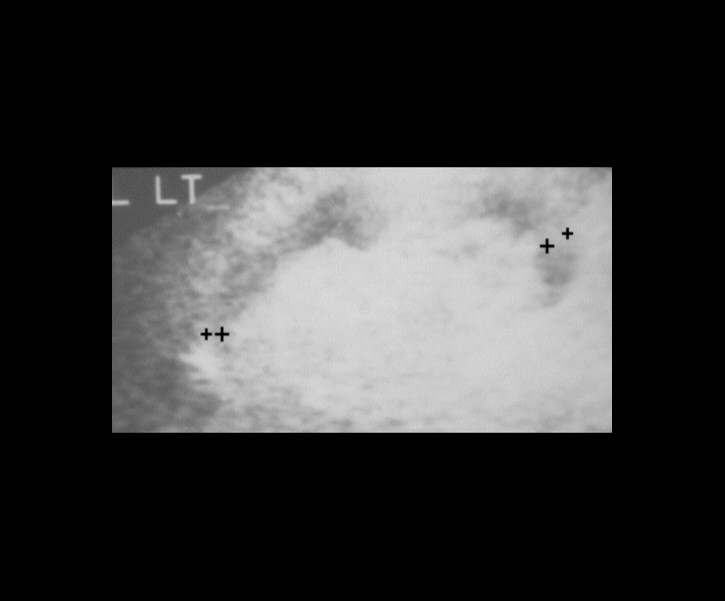
Correct Answer: Renal papillary necrosis
- =NECROTIZING PAPILLITIS = ischemic necrobiosis of medulla (loops of Henle + vasa recta) secondary to interstitial nephritis (interstitial edema) or intrinsic vascular obstruction
Differential Diagnosis:
- mnemonic: "POSTCARD"
- Pyelonephritis
- Obstructive uropathy
- Sickle cell disease
- Tuberculosis, Trauma
- Cirrhosis = alcoholism, Coagulopathy
- Analgesic nephropathy
- Renal vein thrombosis
- Diabetes mellitus (50%)
Pearls:
- Findings may appear as :
- Ball on tee
- Lobster claw sign
- Signet ring
- Sloughed papilla with clubbed calyx
- TB usually appear with:
- Uneven caliectasis
- Multifocal strictures
- Mural thickening and enhancement
- Later there is hydronephrosis and parenchymal thinning with dystrophic calcifications.
Return Back
Correct Answer Explanation




QUESTION-3:
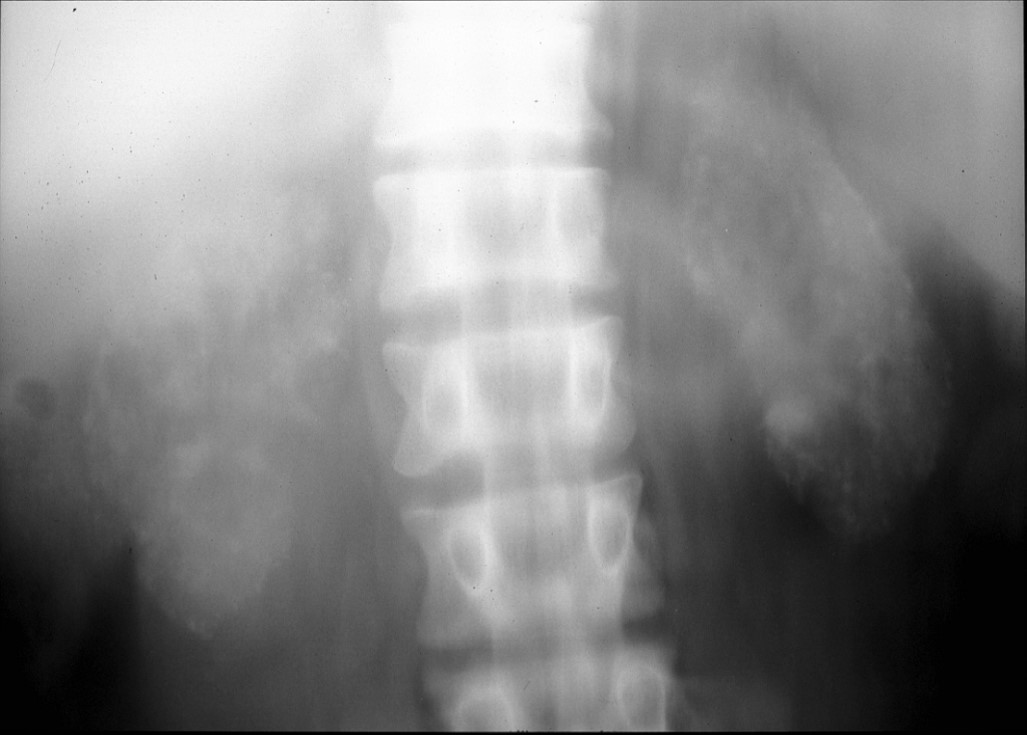
60 yo with back pain:
Correct Answer: Aneurysm
- EXTRARENAL ANEURYSM (2/3)
- Congenital
- Atherosclerotic
- Fibromuscular dysplasia
- Mycotic
- 2.5% of all aneurysms
- Cause:
- bacteremia, SBE, perivascular extension of inflammation
- Organism:
- Streptococcus
- Staphylococcus
- Pneumococcus
- Salmonella
- Neurofibromatosis
- Trauma + renal artery angioplasty
Pearls:
- 1.0-1.5 cm: can be followed
- Follow-up in 1-2 years, if not premenopausal
- >1.5 cm consider surgical
- Aneurysms >2 cm surgical treatment is recommended
Follow-up:
Return Back
Correct Answer Explanation



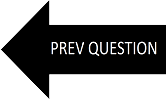
QUESTION-4:
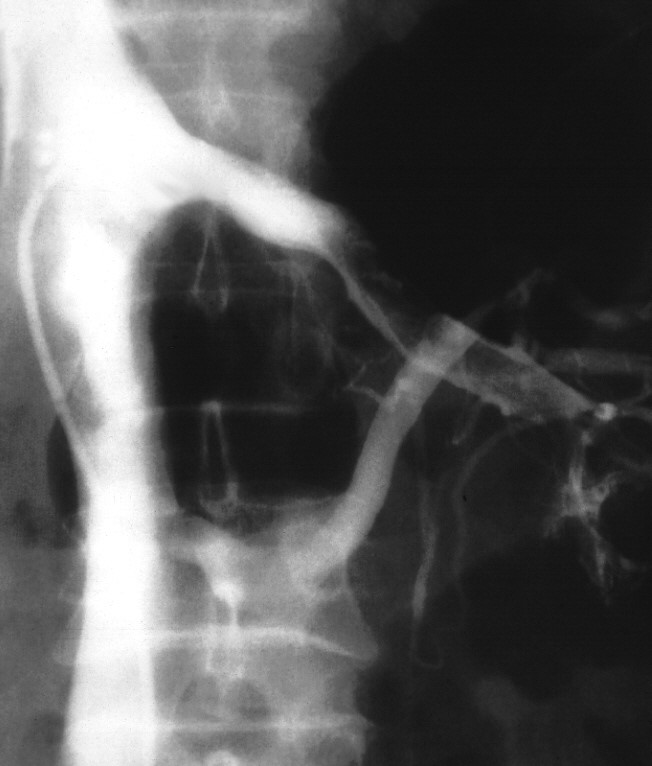
Polyarteritis nodosa:
Correct Answer: Polyarteritis nodosa
- Etiology: Possible deposition of immune complexes.
Differential Diagnosis:
- Necrotizing angiitis, mycotic aneurysm
- Associated with: hepatitis B antigenemia
- Location: all organs may be involved, kidney (85%), heart (65%), liver (50%), pancreas, bowel, CNS (cerebrovascular, accident, seizure)
- Other Sources of Vasculitis - Syphilis, Takayasu, Kawasaki, fungal, TB, polyarteritis nodosa.
Pearls:
- Kidney (most frequently affected organ)
- Multiple small intrarenal aneurysms (interlobar, arcuate, interlobular arteries)
- Aneurysms may disappear (thrombosis) or appear in new locations
- Arterial narrowing + thrombosis (chronic stage/healing stage)
- Multiple small cortical infarcts
Cx:
- Perinephric/subcapsular hemorrhage (rupture of aneurysm)
- Secondary to aneurysm rupture, organ infarction due to vessel thrombosis, gangrene of fingers/toes
- Rx: Steroids (50% 5-year survival rate)
Return Back
Correct Answer Explanation



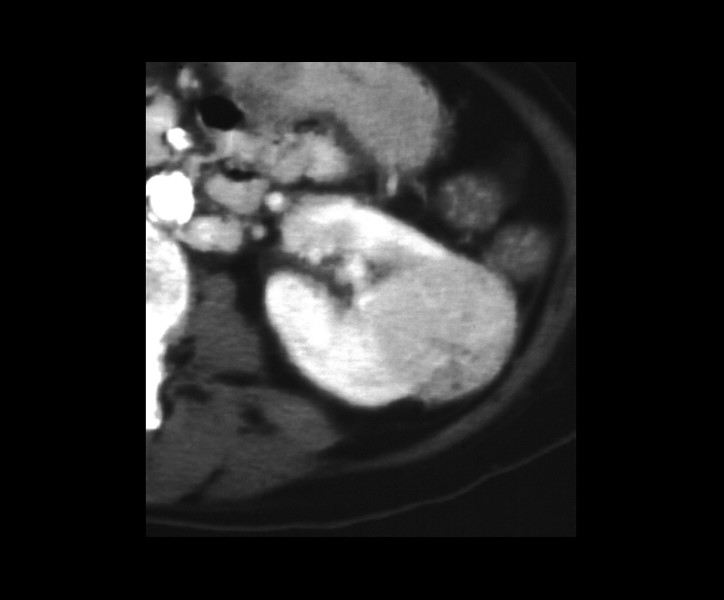
QUESTION-5:
45 yo diabetic patient:
Correct Answer: Renal vein thrombus
- Renal vein thrombosis; "bland" thrombus or tumor thrombus (tumor extending into into the vein).
- mnemonic:"TEST MAN"
- Thrombophlebitis
- Enterocolitis (dehydration)
- Sickle cell disease, Systemic lupus erythematosus
- Trauma
- Membranous glomerulonephritis
- Amyloidosis
- Neoplasm(pancreas, kidney)
Differential Diagnosis:
- RENAL VEIN THROMBOSIS ETIOLOGIES
- “VD STANG”
- Vasculitis
- Dehydration
- SSDz
- Trauma
- Amyloidosis
- Neoplasm
- Glomerulonephritis
Pearls:
- CT angiography is the test of choice for diagnosing RVT; can demonstrate thrombus in the renal vein and, at times, in the vena cava.
- Variable size/enlarged kidney
- Persistent cortical enhancement
- Diminished parenchymal enhancement
References:
- https://bit.ly/2RwedsP
Return Back
Correct Answer Explanation




QUESTION-6:
55 yo man with history of TS:
Correct Answer: Oncocytoma
- Well-encapsulated tan-colored tumor of well-differentiated proximal tubular cells (benign adenoma) + oncocytes
- Majority asymptomatic, occasionally hypertension
- Central stellate scar in 30% (in lesions >3 cm in diameter due to organization of central infarction + hemorrhage after tumor
- Growth has outstripped blood supply)
- Invasion of renal capsule / renal vein in large tumors
Differential Diagnosis:
- Angio:
- Spoke-wheel configuration (80%), homogeneously dense parenchymal phase (71%)
- NO contrast puddling / arteriovenous shunting / renal vein invasion
- NUC:
- Photopenic area (tubular cells do not function normally) on Tc-99m DMSA
- Dx:
- Percutaneous needle biopsy unreliable
- Pathologic diagnosis requires entire tumor because well-differentiated renal cell carcinoma may have oncocytic features!
- Rx:
- Local resection / heminephrectomy
Pearls:
- An oncocytoma is an epithelial cell tumor of the proximal tubule, which has some malignant potential, accounting for 5% of renal tumors. Oncocytomas are impossible to differentiate from RCC by imaging.
- Oncocytoma has similar imaging characteristics with RCC. Look for a central scar on CT or MR or a “spoke wheel” appearance on angiography. Genitourinary Requisites, 89-101, 113-114
RENAL LESIONS TO CONSIDER
- Angiomyolipoma
- Mesoblastic Nephroma
- Multilocular Cystic Nephroma
- Oncocytoma (adenoma)
- RCC
- Hemangiopericytoma - juxtaglomerular
Return Back
Correct Answer Explanation




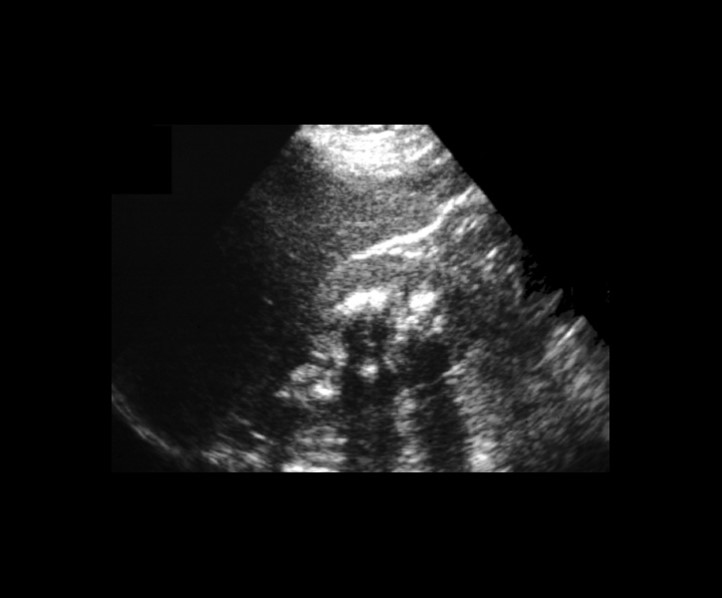
QUESTION-7:
Medullary Nephrocalcinosis:
Correct Answer: Medullary Nephrocalcinosis
- =calcifications involving the distal convoluted tubules in the loops of Henle
- Incidence:95% of all nephrocalcinoses
- mnemonic:"HAM HOP“:
- Hyperparathyroidism
- Acidosis (renal tubular)
- Medullary sponge kidney
- Hypercalcemia / hypercalciuria (sarcoidosis, milk-alkali syndrome, hypervitaminosis D)
- Oxalosis
- Papillary necrosis
- normal-sized / occasionally enlarged kidneys (medullary sponge kidney)
Differential Diagnosis:
- MEDULLARY NEPHROCALCINOSIS “P MOR CAL”
- Papillary necrosis
- Medullary Sponge Kidney (#1, nl to big kidneys)
- Oxalosis
- RTA Type 1 (distal) (diffuse symm calcs w/ nl size kids)
- Ca (chronic ↑ Ca (HPT, etc.)) (small smooth kidneys)
- Analgesic nephropathy (small kidneys)
- Lasix (chronic, in infants)
References:
- https://bit.ly/3ejGKe8
Return Back
Correct Answer Explanation




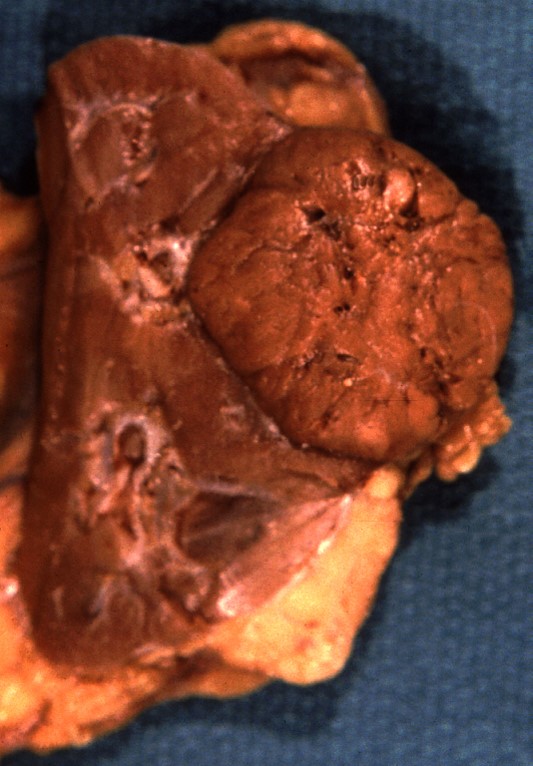
QUESTION-8:
Angiomyolipoma:
Correct Answer: Angiomyolipoma
- Angio: Hypervascular mass (95%) with enlarged interlobar + interlobular feeding arteries, tortuous irregular aneurysmally dilated
- Cx: Hemorrhagic shock from bleeding into angiomyolipoma or into retroperitoneum. Angiomyolipomas >4 cm bleed spontaneously in 50-60%!
- Rx: Annual follow-up of lesions <4 cm. Emergency laparotomy (in 25%): nephrectomy, tumor resection. Selective arterial embolization.
Differential Diagnosis:
- Renal / perirenal lipoma
- Liposarcoma
- Wilms tumor
- AML
- RCC (occasionally contains fat)
Pearls:
- RENAL CHORISTOMA (= benign tumor composed of tissues not normally occurring within the organ of origin)
- =RENAL HAMARTOMA (improper name since fat and smooth muscle do not normally occur within renal parenchyma)
- AML associated with tuberous sclerosis (in 20%)
- AML in 80% of patients with tuberous sclerosis
- commonly large + bilateral + multiple;
- may be the only evidence of tuberous sclerosis
References:
- Genitourinary Requisites, 115, 81-120
Return Back
Correct Answer Explanation
QUESTION-9:
Adult female s/p MVA:
Correct Answer: Intraperitoneal bladder rupture
- Signs of bladder rupture in a patient with a history of trauma include suprapubic tenderness and hematuria. Susceptibility to bladder injury varies with the fullness of the bladder at the time of the accident.
- Bladder rupture is classified as follows:
- Type 1: Bladder contusion
- Type 2: Intraperitoneal rupture: a surgical emergency. Often a seatbelt or steering wheel injury. Usually associated with rupture of the dome.
- Type 3: Interstitial injury: incomplete perforation resulting in a mural defect WITHOUT extravasation of contrast. Rare.
- Type 4: Extraperitoneal rupture
- A: simple
- B: complex? rupture of fascial planes so that contrast may be seen in the thigh, scrotal, pelvic, or perineal regions - Type 5: Combined intra- and extraperitoneal rupture. May see only one type on cystography.
Pearls:
- Extraperitoneal rupture is the most common type of bladder injury, accounting for ~85% (range 80-90%) of cases.
- Usually the result of pelvic fractures or penetrating trauma.
- Cystography reveals a variable path of extravasated contrast material.
- Treatment is with an indwelling Foley catheter.
- Fluoroscopic cystography is the exam of choice to diagnose bladder rupture due to blunt trauma. CT is also an excellent choice if enough contrast is administered to achieve bladder distension. False negatives may occur in cases of penetrating injury.
References:
- https://bit.ly/3zYzU5R
Return Back
Correct Answer Explanation